ORIGINAL
Periodontal status in people with HIV in the municipality of Pinar del Río
Estado periodontal en personas con VIH en el municipio Pinar del Río
Ivette Cáceres González1 ![]() *, Leyda Yenima Pérez Hernández1
*, Leyda Yenima Pérez Hernández1 ![]() , Danisbel Pérez Ayala2
, Danisbel Pérez Ayala2 ![]() , Dunia Milagros Labrador Falero3
, Dunia Milagros Labrador Falero3 ![]() , Jadier Wong Silva4
, Jadier Wong Silva4 ![]()
1Clínica Estomatológica Docente “Antonio Briones Montoto”. Pinar del Río, Cuba.
2Clínica Estomatológica Docente San Juan y Martínez. Pinar del Río.
3Universidad de Ciencias Médicas. Pinar del Río, Cuba.
4Universidad de Ciencias Médicas de Pinar del Río. Hospital Pediátrico Provincial Docente “Pepe Portilla”. Pinar del Río, Cuba.
Cite as: Cáceres González I, Pérez Hernández LY, Pérez Ayala D, Labrador Falero DM, Wong Silva J. Periodontal status in people with HIV in the municipality of Pinar del Río. Odontologia (Montevideo). 2024; 2:121. https://doi.org/10.62486/agodonto2024121
Submitted: 02-02-2024 Revised: 13-05-2024 Accepted: 04-08-2024 Published: 05-08-2024
Editor: Nairobi
Hernández Bridón ![]()
ABSTRACT
Introduction: infection by the human immunodeficiency virus (HIV) reduces the functionality of the immune system and favors the appearance of different pathologies, including periodontal disease.
Objective: to characterize periodontal disease in people living with HIV.
Methods: an analytical observational cross-sectional study was conducted in people living with HIV during the period 2022-2023. The universe included patients living with HIV in the municipality of Pinar del Río (N=381). The sample (non-probabilistic intentional), included 350 patients according to inclusion criteria. The revised Russell’s Oral Hygiene and Periodontal indices were used. For the statistical analysis, absolute and percentage frequencies were used, in addition to the inferential calculation of X2, contingency coefficient, confidence interval and relative risk.
Results: the presence of periodontal disease and advanced gingivitis stood out. Men between 35 and 49 years of age predominated. The most affected by periodontal disease were male patients aged 60 years and older. The most observed risk factors were dentobacterial plaque and the presence of calculus. Poor oral hygiene prevailed, followed by regular in patients with periodontal disease. The sample was characterized by a predominance of asymptomatic patients. In the presence of periodontal disease, severe and advanced stages increased.
Conclusions: significant statistical association of periodontal status with age, sex, oral hygiene and clinical stages of HIV infection was identified.
Keywords: Periodontal Disease; HIV; AIDS; Risk Factors; Oral Pathologies; Periodontitis.
RESUMEN
Introducción: la infección por el virus de la inmunodeficiencia humana (VIH), reduce la funcionalidad del sistema inmunitario y favorece la aparición de distintas patologías, entre ellas, la enfermedad periodontal.
Objetivo: caracterizar la enfermedad periodontal en personas viviendo con VIH.
Métodos: se realizó un estudio observacional analítico, de corte transversal en personas viviendo con VIH durante el período 2022–2023. El universo incluyó pacientes viviendo con VIH en el municipio de Pinar del Río (N=381). La muestra (intencional no probabilística), abarcó a 350 pacientes según criterios de inclusión. Se utilizaron los índices revisados de Higiene bucal y Periodontal de Russell. Para el análisis estadístico se emplearon frecuencias absolutas y porcentuales, además del cálculo inferencial de X2, coeficiente de contingencia, intervalo de confianza y riesgo relativo.
Resultados: resaltó la presencia de enfermedad periodontal y gingivitis avanzada. Predominaron los masculinosde 35 a 49 años. Los más afectados por enfermedad periodontal fueron pacientes masculinos de 60 y más años.
Los factores de riesgo más observados fueron la placa dentobacteriana y presencia de cálculos. Prevaleció mala higiene bucal, seguida de regular en pacientes con enfermedad periodontal. La muestra se caracterizó por predominio de pacientes asintomáticos. En presencia de enfermedad periodontal, aumentaron los estadíos graves y avanzados.
Conclusiones: se identificó asociación estadística significativa del estado periodontal con la edad, sexo, higiene bucal y estadios clínicos de la infección por VIH.
Palabras clave: Enfermedad Periodontal; VIH; SIDA; Factores de Riesgo; Patologías Bucales; Periodontitis.
INTRODUCTION
Periodontopathies are a group of diseases located in the gum and supporting structures of the tooth (ligament and alveolar bone). Chronic periodontal diseases are caused by bacteria from subgingival plaque.(1)
Chronic inflammatory periodontal disease (CIDP) is associated with several risk factors that can initiate and aggravate it. The World Health Organization has described the five most associated risk factors: the microflora of the gingival sulcus, diabetes mellitus, genetic conditions, smoking, and stress.(2)
The human immunodeficiency virus (HIV/AIDS) is an RNA virus that consists of a lipid envelope and a central nucleocapsid inside which the genetic material and enzymes necessary for its life cycle are located. HIV has a tropism towards mononuclear cells such as TCD4+ lymphocytes, macrophages, and Langerhans cells as they commonly express the surface CD4 receptor and HIV co-receptors (CXCR4 and CCR5).(3)
HIV within the oral cavity may influence the predisposition to specific periodontal pathology. Periodic follow-up and strict control of the periodontal status are necessary to avoid the appearance of new pathologies. It would be important to pay special attention to the immunological and virological parameters of the patients since they provide information on the systemic status.(4)
Some factors imply a higher risk of developing periodontitis or other oral lesions. The appearance of oral lesions, such as severe forms of gingivitis and periodontitis, may be an indication that a patient is HIV-infected.(4,5)
Periodontal diseases in HIV seropositive patients include the conventional forms of gingivitis, periodontitis, and alterations produced by bacterial, fungal, and viral infections. This condition’s clinical significance is associated with severe suppression of the immune system with CD4 cell counts below 100 cells/mm.(6)
An effective clinical oral examination can determine the first manifestations of infection in people living with HIV since the mouth is usually one of the areas in which it is possible to identify the first signs of infection and, in the course of the disease, will appear at least one alteration in it. Periodontal lesions associated with HIV/AIDS infection are the most frequent.(6)
These lesions may be present in up to 50 % of people with HIV infection and 80 % of people with a diagnosis of AIDS. The prevalence of periodontal disease is high in people living with HIV in Latin America, where the epidemic is estimated to have begun in the early 1980s. Chorley(7) and Andagoy(8) cite a significant percentage, between 60 and 72 %, with the United States, Brazil and Chile having the highest incidence.
HIV was detected in Cuba in 1986; the target city was Havana, which has managed to maintain a low HIV growth rate and constitutes an exception in the Caribbean area with a prevalence below 0,1 % in adults. The epidemic is characterized by concentrated, slow growth and minimal incidence of this infection in the child population.(9)
In Cuba, the prevalence of periodontal disease in people living with HIV is described as ranging between 70 and 78,3 %. The HIV/AIDS epidemic in Pinar del Río province has maintained an increasing trend since its beginning in 1986, with a total of 972 people living with HIV diagnosed by the end of 2021, of which 52,8 % are concentrated in the municipality of Pinar del Río, which is considered one of the highest risk municipalities in the province and the country.(9,10)
Taking into account that there are few studies carried out in the province related to the periodontal status of people living with HIV and that there are no studies after the introduction of antiretroviral treatment to all those infected by this virus in 2015, this research was conducted to characterize the periodontal status in people living with HIV residing in the municipality of Pinar del Río.
METHOD
An analytical observational cross-sectional study was carried out to characterize the periodontal status of people living with HIV residing in the municipality of Pinar del Río between January 2022 and September 2023 at the “Antonio Briones Montoto” Stomatological Clinic and health areas belonging to the Provincial Center of Hygiene Epidemiology and Microbiology, (Polyclinics: “Hermanos Cruz,” “Pedro Borras”, “Turcios Lima” and “Raúl Sánchez”), for the planned serological control.
The universe included all patients living with HIV in the municipality of Pinar del Río (N=381). The sample (non-probabilistic intentional) was formed by 350 patients, taking into account that they were those diagnosed with HIV, received the ambulatory care service, and were willing to participate in the research.
Patients with total edentulism were excluded, as well as those with insufficient or no documentary evidence to obtain the necessary data for the research.
The following variables were used: periodontal clinical status, presence of periodontal disease, age, sex, local action factors, oral hygiene, and clinical stage of HIV infection.
Data collection techniques
A thorough interrogation and oral examination of the study population were conducted using a classification set (mirror, forceps, and explorer) and a periodontal probe. The Periodontal Clinical History and the information collection form elaborated by the researcher where variables of interest for the study were collected.
To describe the severity of periodontal disease, the revised WHO Russell Periodontal Index was used, which has been frequently used in Cuba and handles the most obvious signs of the disease, such as inflammation, pocket formation, and tooth mobility.(11)
The revised oral hygiene index (IHB-R) was used to evaluate the quality of oral hygiene in patients, where only the tooth surface with the worst hygiene was rated as a record.(11)
Data processing and analysis techniques
An Excel database for Windows was created to process the information. The process was carried out using the SPSS version 19 software package, and the results were presented in statistical tables and graphs.
The statistical data were organized and summarized in contingency tables, and descriptive tools such as frequency distribution and percentage calculation were used. The nonparametric Chi-square test (X²) was applied, with a significance level α=0,05 to determine the significant association or not between 2 qualitative variables, as well as the statistical tests contingency coefficient (CC) to determine the factors most associated with the presence of periodontal disease, the confidence interval (CI) to calculate the proportion for a 95 % confidence interval and the calculation of the relative risk (RR) for some selected variables.
Ethical aspects
Fundamental ethical principles were complied with while searching for and collecting data for the research. The confidentiality of the information obtained was guaranteed, and it was to be used only for teaching and research purposes.
Informed consent to participate in the study was officially requested, with the authorization of the Scientific Councils and Directors of the “Antonio Briones Montoto” Stomatological Clinic and Health Areas belonging to the Provincial Center of Hygiene, Epidemiology, and Microbiology.
RESULTS
Table 1 shows a predominance of 288 people with periodontal disease for 82,3 %.
|
Table 1. Periodontal status of people living with HIV. Pinar del Río, 2022-2023 |
||
|
Presence of periodontal disease |
No. |
% |
|
With periodontal disease |
288 |
82,3 |
|
Without periodontal disease |
62 |
17,7 |
|
Total |
350 |
100 |
Table 2 shows a predominance of advanced gingivitis, with 128 affected, representing 36,6 % of the population studied. The statistical analysis shows a proportion between 31,5 and 41,6 for the 95 % confidence, thus demonstrating that the most frequently presented conditions affected the protective periodontium. These pathologies can appear in both HIV seropositive and seronegative patients. When calculating the relative risk value (RR) between the healthy group and those with periodontal disease, it was shown that 4 out of every 100 people are at risk of suffering from periodontal disease.
|
Table 2. Severity of periodontal disease in people living with HIV |
|||||
|
Severity of periodontal disease |
Russell Index |
No. |
% |
IC 95 % |
|
|
With periodontal disease |
Mild gingivitis |
1 |
106 |
30,3 |
25,5-35,1 |
|
Advanced gingivitis |
2 |
128 |
36,6 |
31,5-41,6 |
|
|
Incipient or mild periodontitis |
6 |
48 |
13,7 |
10,1-17,3 |
|
|
Advanced periodontitis |
8 |
6 |
1,7 |
0,4-3,1 |
|
|
No periodontal disease |
0 |
62 |
17,7 |
13,7-21,7 |
|
Table 3 shows a predominance of the 35 to 49 age group (39,1 %) and male sex (96,1 %). Of the total number of people living with HIV, the group aged 60 years and over stood out, where all (100 %) had periodontal disease. There was a gradual increase in the proportion of periodontal disease according to age, but the biggest jump was seen after 24 years.
The results of the nonparametric statistical test X2 (p<α α=0,05) showed a significant statistical relationship between the presence of periodontal disease and the variables age and sex.
|
Table 3. Periodontal status of the studied sample according to age and sex |
||||||
|
|
With periodontal disease |
No periodontal disease |
Total |
|||
|
No. |
% |
No. |
% |
No. |
% |
|
|
Sex |
|
|
|
|
|
|
|
Male |
271 |
96,1 |
11 |
3,9 |
282 |
80,6 |
|
Female |
17 |
25,0 |
51 |
75,0 |
68 |
19,4 |
|
X2 =190,0; G.L.=1; P=0; Contingency Coefficient (CC=0,59) Relative Risk (RR: 4,2) |
||||||
|
Age groups (years) |
||||||
|
15-19 |
0 |
0 |
2 |
100 |
2 |
0,6 |
|
20-24 |
11 |
64,7 |
6 |
35,3 |
17 |
4,9 |
|
25-34 |
72 |
75 |
24 |
25 |
96 |
27,4 |
|
35-49 |
112 |
81,8 |
25 |
18,2 |
137 |
39,1 |
|
50-59 |
59 |
92,2 |
5 |
7,8 |
64 |
18,3 |
|
60 y + |
34 |
100 |
0 |
0 |
34 |
9,7 |
|
Total |
288 |
82,3 |
62 |
17,7 |
350 |
100 |
|
X2 =28,04; G.L.=5; P=0; CC=0,27 |
||||||
The most frequent risk factors in the studied population with periodontal disease, shown in figure 1, were antibacterial plaque 83,7 % and the presence of calculus (70,6 %). According to the results of the non-parametric statistical test X2 (p<α α=0,05) X2, a significant statistical association was confirmed for exposure to risk factors, among which antibacterial plaque (240,5; p=0) and calculus (180,7; p=0) stand out. However, in the case of smoking, which shows values of X2=1,35; p=0,2 (p>α α=0,05), it was confirmed that there is no statistical association between this risk factor and periodontal disease in this study.
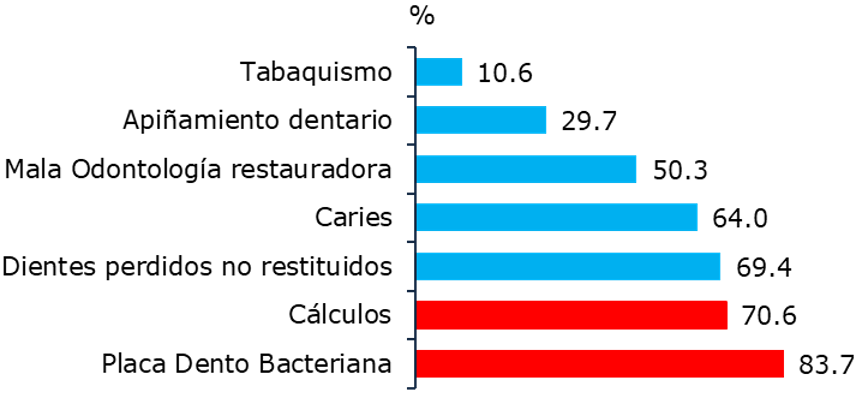
Figure 1. Risk factors associated with the presence of periodontal disease
According to the periodontal status described in table 4, the oral hygiene values showed a significant predominance of poor oral hygiene (100 %) followed by regular oral hygiene (94,7 %) in patients with periodontal disease. The results of the nonparametric statistical test X2 (p<α α=0,05) show a statistically significant relationship between the variables oral hygiene and periodontal disease.
|
Table 4. Oral hygiene according to periodontal status |
||||||
|
Oral hygiene |
With periodontal disease |
No periodontal disease |
Total |
|||
|
No. |
% |
No. |
% |
No. |
% |
|
|
Good |
6 |
10,5 |
51 |
89,5 |
57 |
34,3 |
|
Fair |
198 |
94,7 |
11 |
5,3 |
209 |
41,7 |
|
Poor |
84 |
100 |
0 |
0 |
84 |
24,0 |
|
Total |
288 |
82,3 |
62 |
17,7 |
350 |
100 |
|
X2 =241,7; G.L.=2; P=0; CC=0,64 |
||||||
Table 5 shows a predominance of asymptomatic patients (74,8 %). Severe (100 %) and advanced (92,3 %) clinical stages of infection prevailed in patients with the presence of periodontal disease. This translates into CD4 results below 200 and 100 cells, with evident deterioration of the immune status of these patients, leading to the appearance of opportunistic diseases. From the statistical point of view, a significant statistical association was evidenced between periodontal disease and the clinical stage of HIV infection because X2 (p<α α=0,05).
|
Table 5. Periodontal status according to clinical stage of HIV infection |
||||||
|
Clinical stage |
With periodontal disease |
No periodontal disease |
Total |
|||
|
No. |
% |
No. |
% |
No. |
% |
|
|
Asymptomatic |
208 |
81,3 |
48 |
18,8 |
256 |
74,8 |
|
Mild symptoms |
37 |
75,5 |
12 |
24,5 |
49 |
13,2 |
|
Advanced symptoms |
24 |
92,3 |
2 |
7,7 |
26 |
7,4 |
|
Severe symptoms |
19 |
100 |
0 |
0 |
19 |
4,6 |
|
Total |
288 |
82,3 |
62 |
17,7 |
350 |
100 |
|
X2 =9,62; G.L.=3; P=0,02; CC=0,16 |
||||||
DISCUSSION
The prevalence of periodontal disease increases when the individual is infected by HIV/AIDS because there is immunosuppression and susceptibility to opportunistic infections that alter the response of periodontal tissues.(4)
Among the manifestations that may appear in patients with HIV/AIDS infection, oral cavity lesions are of great relevance. Studies around the world indicate that these lesions may be present in up to 50 % of people with HIV infection and 80 % of people diagnosed with AIDS. The differences in percentage are due to the variety of investigations, methodologies, types of studies, epidemiological heterogeneity, demographic region, and type of therapy the patient is receiving.(6)
The similarity is found with what is observed in table 1, with the research conducted in Ecuador by Grijalva Palacios et al.(12), where a high prevalence of periodontal disease is obtained in people living with HIV.
These results differ from those found in the research conducted by Loredo Sandoval et al.(1), highlighting the predominance of healthy patients, with 54,5 % of the population not having periodontal disease.
Jampani(13) confirms the association between PI-R and the degree of immunity. The greater the deterioration of immunity, the higher the values of the periodontal index.
Similar results were found in the research conducted in Mexico by Chorley Sanchez et al.(7) related to oral lesions in people living with HIV, where the most frequent periodontal condition was gingivitis and was present in 40,5 % of the population studied.
In a systematic review study conducted by Grijalva Palacios et al.(12), the scientific evidence analyzed reflects different data: predominance of periodontal disease, followed by candidiasis, oral ulcers, and gingivitis in fourth place of prevalence.
In the present investigation, it was found that age ≥ 30 years constitutes a risk factor for presenting periodontal disease.
Authors such as Pérez Barrero(14) and Fonseca(15) think that the prevalence of periodontal disease increases with age, and in general, one should expect to find a higher prevalence in older adults. Rather than indicating increased susceptibility to periodontitis in the elderly, this age effect could represent the cumulative effect of prolonged exposure to true risk factors.
Marín and Duque(5) state that age has been one of the most studied modifying conditions of periodontal disease since it is a variable analyzed in almost all epidemiological studies.
Different authors(14,15,16) have shown in their research that periodontal disease appears around 20 years of age, increases with age, a large part of the population is affected by some form of mild or moderate periodontopathy, and some percentage presents more severe forms.
Chorley Sanchez et al.(7) conducted a cross-sectional analysis in 161 Mexican men to determine the prevalence, severity, and extent of chronic periodontitis associated with several factors, among them age, which showed that being older than 35 years was associated with the appearance of periodontitis (OR=2,08; CI=1,05-4,10).
With different results, Sánchez Artigas et al.(2), when applying the X2 test and univariate analysis, concluded that age did not show a statistically significant effect (p=0,5200) despite obtaining OR values higher than 1: 45-54 years: OR=1,76; 95 % CI: [0,65-4,76] 55-64 years: OR=1,2486 95 % CI: [0,49-3,13].
Regarding the sex variable, the results obtained by Rojo Botello et al.(16) were similar to those found in the present study regarding male predominance. These authors reported a high prevalence of oral lesions in the study population, with a high incidence in men.
Some authors state that the male sex has 4,2 times more risk of contracting periodontal disease than the female sex because they consider that women demand more stomatological attention due to esthetic purposes, which includes cleaning the oral cavity so that periodontal disease in any of its categories shows a tendency to be lower in women than in the opposite sex.(16,17)
Most studies on periodontal disease record better periodontal status in women than in men, which is also associated with the statement that this sex is the most affected by HIV/AIDS, according to national and international figures.(7,16,17)
Other similar results were found by Marín and Duque(5), where it is stated that sex seems to be an important variable in periodontitis. Pavón Zepeda et al.(18) report different results, with predominance in the female sex.
In the present study, the influence of dental plaque on periodontal disease was demonstrated, which coincides with what is described in the literature, where it is stated that bacterial plaque located on dental surfaces favors the development of gingivitis, which is the first stage of most forms of periodontal disease. This is a modifiable risk factor through health promotion and prevention strategies to prevent periodontal disease development and progression.(15,18)
The authors consider that the increase in periodontal disease has been gradual according to the quality of oral hygiene presented by the population studied. However, the biggest jump is seen from before to after the regular condition, demonstrating that regular oral hygiene produces a high effect in the increase of the probability of presenting periodontal disease; this statement is equally valid for poor oral hygiene concerning regular oral hygiene.
The risk of contracting periodontal disease increases when the individual is immunocompromised and has opportunistic infections that alter the response of periodontal tissues. People living with HIV are more susceptible to periodontal disease, even more so if the patient has poor oral hygiene and no medical care until very advanced stages of the condition.(2,15,18,19)
Oral hygiene is the most important risk factor in the origin and evolution of periodontopathies; when it is deficient, bacterial plaque accumulations are created, and as we age, its microbial content changes towards more pathogenic forms. If they are not eliminated, they calcify and cause calculus, which, being hard, irritating, and rough, retains more bacterial plaque. Periodontal disease is a direct consequence of poor oral hygiene. Interdental hygiene methods significantly reduce plaque rates and improve gingivitis.(19,20)
Different investigations refer to the presence of periodontal disease in HIV-infected persons and take as a starting point the lack of good oral hygiene practices as the main error of the patients. Several international organizations address the importance and benefits of developing activities that promote oral health.(3,4,19,20)
Among the risk factors studied, poor oral hygiene ranked first, which coincides with the literature consulted, which refers to this factor as the most important. Bacterial accumulation favored by poor oral hygiene aggravates periodontal disease.(19,20)
Deficient oral hygiene is a factor traditionally related to the presence of caries and periodontal disease. However, it is known to be related to all oral diseases as a predisposing or aggravating factor. Adequate oral hygiene directly eliminates microorganisms adhered to the dental surfaces, preventing or limiting their harmful effects.(19,20)
Similar findings are found by Fonseca Vázquez(15), who states that poor oral hygiene was the predominant risk factor since, in most patients, there was abundant debris and calculus and concludes that poor oral hygiene increased the risk of suffering from chronic periodontitis five times more than in those who practiced proper oral hygiene (OR=5,693; 95 % CI: [2,54-12,73]; p=0,0000).
Under normal conditions, the oral mucosal epithelium plays an important role in protecting the host against pathogens that cause infections. However, in patients with HIV/AIDS infection, the oral epithelium undergoes molecular alterations that increase susceptibility to infection.(6)
Despite the effectiveness of anti-retroviral therapy (ART) in increasing CD4 T-lymphocyte count, complete immune recovery of oral mucosal epithelial cells is not achieved, a degree of susceptibility to infectious agents persists, and even a degree of vulnerability to the toxic effects of anti-retroviral drugs is generated.(6)
The massive introduction of ART has not only reduced the morbidity and mortality of classic opportunistic complications but has also modified their frequency, type of clinical manifestations, and time of onset. It is important to understand that oral lesions caused by opportunistic agents occur in patients with HIV/AIDS infection, whether or not they are on ART.(21,22)
Although the occurrence of some lesions classically associated with HIV infection, such as Kaposi’s sarcoma, hairy leukoplakia, periodontal disease, and mucosal ulcerations, has decreased with the introduction of ART, other conditions, such as oropharyngeal candidiasis, have remained constant. In contrast, papillomatous lesions and salivary gland pathology have increased.(21,22)
The presence of oral lesions continues to be significant as they may indicate a deterioration of the patient’s immune system and are considered early markers of disease. They may also be associated with decreased CD4 T-lymphocyte count and increased viral load.(21,22)
It has been described in the literature that in patients who did not suffer from the periodontal disease at the time of infection, they suffered from it during the infection in its different stages and that it worsened with the decrease of TCD4+ cells and the appearance of other major opportunistic diseases.(4,6)
A directly proportional relationship is established between the risk factor and the presence of the disease, i.e., if the influence of the factor decreases, the disease improves. The factor under analysis cannot be eliminated because once the patient is infected, the disorder is irreversible, but if the clinical and immunological conditions are improved, the oral lesions improve and, therefore, the periodontal disease; such is the case that when the viral load decreases, and the CD4+ T cell count increases, the clinical characteristics and the evolution of the patient with inflammatory periodontal disease improve.(2,5,6,15)
The results of this research are similar to the literature consulted(2,15,18,19), where it is stated that the more severe the clinical diagnosis of HIV/AIDS, the more generalized and aggravated the periodontitis is, and the more it is related to the inadequate immunological response of the periodontium to the aggression of microorganisms and their products, finding similarities with this study.
In patients with HIV/AIDS, in whom there is a progressive immunodeficiency, an alarming loss of superficial and deep tissues of the periodontium is observed without a proportional dependence on the accumulation of antibacterial plaque; that is, these processes usually occur in hygienic mouths.(3,4)
The periodontal-pathogenic flora of these patients is not very different from that of HIV-negative patients. Therefore, the alarming clinical signs seen in patients with HIV/AIDS infection are mainly due to the reduced immune capacity or resistance in these cases.(3,4)
Immunodeficiencies are undoubtedly a risk factor for periodontitis due to the complex interaction between cellular and humoral mechanisms; also, the regulation of immune function is excellently adjusted, and therefore, it is likely that sensitivity to periodontitis is determined with the imbalance in the regulatory immune function.(4,6,7)
Recent studies explain the immune system’s role in initiating and exacerbating inflammatory periodontal disease. However, there are few reviews about the possible mechanisms of association of human immunodeficiency virus (HIV) infection with inflammatory periodontal disease. Given the compromise of the patient’s immune system, HIV infection may be a risk factor in the pathogenesis of PID.(4,6,7)
Some researchers state that as the time from diagnosis increases, the percentage of patients with periodontal disease increases since they would be more affected by the factors that influence this condition, such as age, sex, risk factors of local action, as well as the clinical stage of HIV infection, viral replication, concomitant diseases, complexity of therapy, among others.(4,6,7)
From the results obtained in the present investigation, it is concluded that a significant statistical association of periodontal status with age, sex, oral hygiene, and clinical stages of HIV infection was identified.
REFERENCES
1. Loredo Sandoval Y, Cruz Morales R, Cazamayor Laime Z, Montero Arguelles M. Comportamiento de la enfermedad periodontal inmunoinflamatoria crónica. Jovellanos. Matanzas. Rev. Med. Electrón. [Internet]. 2019 [citado 12/06/2024]; 41(1): 78-89. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1684-18242019000100078&lng=es
2. Sánchez Artigas R, Sánchez Sánchez RJ, Sigcho Romero CR, Expósito Lara A. Factores de riesgo de enfermedad periodontal. Correo Científico Médico. [Internet] 2021 [citado 12/06/2024]; 25(1): [aprox. 18 p.]. Disponible en: https://www.medigraphic.com/pdfs/correo/ccm-2021/ccm211p.pdf
3. Cajape González AL, Cano Alvarado AM, Saltos Pincay KN. Virus de la Inmunodeficiencia Humana (VIH) efectos y complicaciones adquiridas durante la infección. Higía [Internet]. 2022 [citado 12/06/2024];7(2). Disponible en: https://revistas.itsup.edu.ec/index.php/Higia/article/view/750
4. Cruz Pérez JL, Olivera Martínez O, Estrada Mirabal Y. Infecciones oportunistas orales asociadas al virus de inmunodeficiencia humana. Mayabeque: I Forum Científico Virtual Ciencias Mayabeque 2021. [Internet]. 2021. [citado 12/06/2024]; e20. Disponible en: http://www.cienciamayabeque2021.sld.cu/index.php/Fcvcm/Cienciamayabeque2021/paper/viewFile/95/156
5. Marín Jaramillo R, Duque Duque A. Condiciones modificadoras del riesgo de enfermedad periodontal: una revisión narrativa sobre la evidencia en américa latina. CES odontol. [Internet]. 2021 [citado 12/06/2024]; 34(1): 82-99. Disponible en: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-971X2021000100082&lng=en
6. Turriate Vivar C, Rodríguez Flores A, Castro Rodríguez Y. Asociación entre los niveles de linfocitos T CD4 y lesiones bucales de portadores del VIH/sida. Rev. Cubana Estomatol, [Internet]. 2021 [citado 12/06/2024]; 58(2): e16. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75072021000200006&lng=es.
7. Chorley Sánchez J, Nájera Ortiz JC. Lesiones en cavidad oral en pacientes con VIH en un estado del sur de México. Odontol Sanmarquina [Internet]. 2019 [citado 12/06/2024]; 22(1):13-8. Disponible en: https://revistasinvestigacion.unmsm.edu.pe/index.php/odont/article/view/15838
8. Andagoya Murillo JM, Zambrano Vera DR, Alcívar Vera CI, Patiño Zambrano VP. Perfil Epidemiológico del VIH en Latinoamérica. RECIMUNDO: Revista Científica de la Investigación y el Conocimiento. [Internet]. 2019 [citado 12/06/2024]; 3(1): 232-58. Disponible en: https://dialnet.unirioja.es/descarga/articulo/6796772.pdf
9. Soto Camejo C, Camejo Pérez C, Soto Martínez O, Matos Jarrosay A, Luciano Aguilar D. Caracterización de la infección por VIH/sida en el municipio Guantánamo. Rev. inf. cient. [Internet]. 2021 [citado 12/06/2024]; 100(2): e3309. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1028-99332021000200002&lng=es.
10. García Alúm N, Chirino Labrador D, Rivero Cruz Y, Paredes Díaz R, Gutiérrez García L. Adherencia terapéutica antirretroviral en pacientes con VIH/SIDA pertenecientes al Policlínico Pedro Borras. Universidad Médica Pinareña [Internet]. 2022 [citado 12/06/2024]; 18(S1): e13. Disponible en: https://revgaleno.sld.cu/index.php/ump/article/view/923
11. Pérez Ayala D, Labrador Falero DM, Martínez Pita M, Cáceres González I. Enfermedad periodontal inmunoinflamatoria crónica en pacientes diabéticos. Rev Ciencias Médicas [Internet]. 2023 [citado 12/06/2024]; 27(1): e13. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1561-31942023000100014&lng=es.
12. Grijalva Palacios MM, Ponce Reyes NS, Vásquez Guerra NL. Diferencias entre las manifestaciones orales en niños, adolescentes y adultos con VIH/SIDA. Gac méd estud [Internet]. 2023 [citado 12/06/2024]; 5(1): e192. Disponible en: https://revgacetaestudiantil.sld.cu/index.php/gme/article/view/192
13. Jampani ND, Sunkavilli RK, Songa VM, Buggapati L, Pathagunti SR. Periodontal health status among HIV-seropositive pregnant women. Indian Journal of Dental Research. [Internet]. 2019 [citado 12/06/2024]; 30(4): 521-6. Disponible en: http://journals.lww.com/ijdr/fulltext/2019/30040/periodontal_health_status_among_hiv_seropositive.9.aspx
14. Pérez Barrero BR, Ortiz Moncada C, DuharteGarbey C, Sánchez Zapata R. Severidad de la periodontitis crónica en el adulto mayor. Medimay [Internet]. 2020 [citado 12/06/2024]; 27(2): [aprox. 9 p.]. Disponible en: http://revcmhabana.sld.cu/index.php/rcmh/article/view/1646
15. Fonseca Vázquez M, Ortiz Sánchez Y, Martínez Sánchez N, Rosales Ortiz A, Proenza Pérez D. Factores de riesgo asociados a la periodontitis crónica en pacientes adultos. Multimed. [Internet]. 2021 [citado 12/06/2024];25(6): e12. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1028-48182021000600003
16. Rojo Botello N, Flores Espinoza A, Arcos Castro M. Prevalencia, severidad y extensión de periodontitis crónica. Scielo Revista Odonto. Mex. [Internet] 2020 [citado 12/06/2024]; [aprox. 10 p.]. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1870-199X2011000100006
17. Ramos Calás M, Ramos Bermúdez J, Fontaine Machado O. Periodontopatías en pacientes del área de salud del policlínico Dr. Gustavo Aldereguía Lima, Las Tunas. Revista Electrónica Dr. Zoilo E. Marinello Vidaurreta [Internet]. 2022 [citado 12/06/2024]; 47(6): e7. Disponible en: https://revzoilomarinello.sld.cu/index.php/zmv/article/view/3180
18. Pavón Zepeda SR, Ochoa Martínez RE, Carrillo Toledo MG, Capetillo Hernández G, Tiburcio Morteo L, Torres Capetillo E, et al. Detección de enfermedades periodontales mediante el índice de Russell en pacientes geriátricos de Omealca, Veracruz. Rev. Mex. Med. Forense. [Internet]. 2020 [citado 12/06/2024]; 5(suppl 3): 29-32 Disponible en: https://revmedforense.uv.mx/index.php/RevINMEFO/article/view/2822/4723
19. Moreno Abello GC, Lara Hernández LC. Caries dental: de la placa ecológica a las decisiones clínicas. Universitas Odontológica. [Internet]. 2020 [citado 12/06/2024]; (39): e46. Disponible en: https://revistas.javeriana.edu.co/index.php/revUnivOdontologica/article/view/28933/24807
20. Labrada Fonseca M, Boduet Vargas D, Labrada Rodríguez M, Campo Álvarez A. Gingivitis crónica: asociación con sexo, higiene bucal y depresión. Revista científica estudiantil 2 de diciembre [Internet]. 2022 [citado 12/06/2024]; 5(2): e14. Disponible en: http://revdosdic.sld.cu/index.php/revdosdic/article/view/313
21. Pérez Bastán JE. Adherencia al tratamiento antirretroviral de personas con VIH/sida en la Atención Primaria de Salud. Rev. Haban. Cienc. Méd. [Internet]. 2020 [citado 12/06/2024]; 19(5): e19. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1729-519X2020000600011&lng=es.
22. Reyes Ríos LÁ, Campo Torregroza E, Espinosa Aguilar A, Granados Pérez A, Gil Ruiz ID. Adherencia al tratamiento antirretroviral en personas con VIH/sida de la región Caribe - colombiano. Rev. Cubana Hig. Epidemiol. [Internet]. 2020 [citado 12/06/2024]; 57: e15. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1561-30032020000100013&lng=es.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
FUNDING
No funding was received for this study.
AUTHORSHIP CONTRIBUTION
Conceptualization: Ivette Cáceres González, Leyda Yenima Pérez Hernández, Danisbel Pérez Ayala, Dunia Milagros Labrador Falero, Jadier Wong Silva.
Data curation: Ivette Cáceres González, Leyda Yenima Pérez Hernández, Danisbel Pérez Ayala, Dunia Milagros Labrador Falero, Jadier Wong Silva.
Formal analysis: Ivette Cáceres González, Leyda Yenima Pérez Hernández, Danisbel Pérez Ayala, Dunia Milagros Labrador Falero, Jadier Wong Silva.
Research: Ivette Cáceres González, Leyda Yenima Pérez Hernández, Danisbel Pérez Ayala, Dunia Milagros Labrador Falero, Jadier Wong Silva.
Writing - original draft: Ivette Cáceres González, Leyda Yenima Pérez Hernández, Danisbel Pérez Ayala, Dunia Milagros Labrador Falero, Jadier Wong Silva.
Writing - proofreading and editing: Ivette Cáceres González, Leyda Yenima Pérez Hernández, Danisbel Pérez Ayala, Dunia Milagros Labrador Falero, Jadier Wong Silva.